Supporting HPC transplant patients can be challenging and confusing to learners.

Dr. Brian Adkins
Let’s clear it all up!
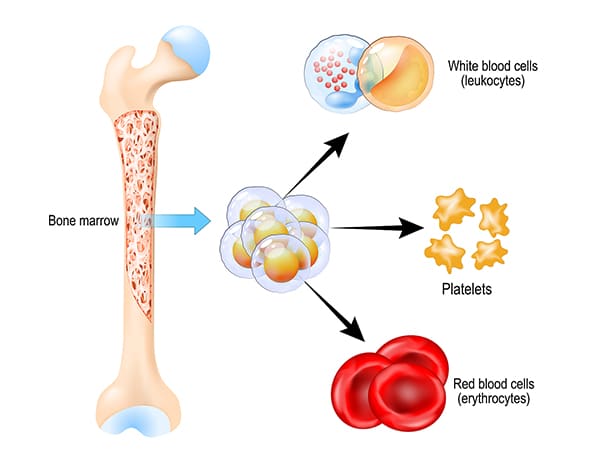
I asked Dr. Brian Adkins, lead author of an excellent review of transfusion before and after HPC transplant (article linked below) to guide us to better understanding, In this episode, Brian discusses things like the different types of stem cell transplants (autologous and allogeneic), the importance of HLA and ABO matching, and the steps involved in collecting and preparing grafts. We also describe the various sources of stem cells (peripheral blood, bone marrow, and umbilical cord blood) and the pros and cons of each. Additionally, Brian addresses practical issues like pre-transfusion testing, the management of ABO incompatible transplants, and the inevitable need for transfusion support during the engraftment period. Near the end, we even describe how to make decisions following an ABO-incompatible HPC transplant.

Dr. Brian Adkins
Let’s clear it all up!
I asked Dr. Brian Adkins, lead author of an excellent review of transfusion before and after HPC transplant (article linked below) to guide us to better understanding, In this episode, Brian discusses things like the different types of stem cell transplants (autologous and allogeneic), the importance of HLA and ABO matching, and the steps involved in collecting and preparing grafts. We also describe the various sources of stem cells (peripheral blood, bone marrow, and umbilical cord blood) and the pros and cons of each. Additionally, Brian addresses practical issues like pre-transfusion testing, the management of ABO incompatible transplants, and the inevitable need for transfusion support during the engraftment period. Near the end, we even describe how to make decisions following an ABO-incompatible HPC transplant.
About My Guest:
Dr. Brian Adkins is an Assistant Professor of Pathology at the University of Texas Southwestern Medical Center. He serves as the Medical Director of Transfusion and Tissue Services at Children’s Health Dallas. He attended medical school at the Joan C. Edwards School of Medicine at Marshall University and completed his Anatomic Pathology/Clinical Pathology residency at Vanderbilt University Medical Center. He went on to complete fellowship training in Blood Banking/Transfusion Medicine and Hematopathology at University of Virginia Health. He is board- certified in Anatomic Pathology and Clinical Pathology with subspecialty certification in Blood Banking/Transfusion Medicine and Hematopathology. His interests include resident and fellow education as well as clinical research.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. Neither Dr. Adkins nor I have any relevant financial disclosures.
Further Reading:
- Excellent review article mentioned in the episode: Adkins BD et al. Transfusion Support in Hematopoietic Stem Cell Transplantation: A Contemporary Narrative Review. Clinical Hematology International 2024;6(1):128-140.
- AABB RBC transfusion guidelines mentioned in episode: Carson JL et al. Red Blood Cell Transfusion: 2023 AABB International Guidelines. JAMA 2023;330(19):1892-1902.
Special thanks to Tommy Walker and Tommy Walker Ministries for the use of his amazing song, “Get Up,” heard at the beginning and end of the episode.
Music Credit
Music for this episode includes “Reflejo” by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














Nice job :). I would suggest that the simplest formula for transfusion is to avoid infusing any ABO antigen (soluble or cellular) that the recipient has circulating antibody to. This is the most dangerous in terms of organ injury, vascular damage and increased bleeding according to current data. Infusing AB or A plasma into an O individual is associated with increased bleeding, sepsis, organ injury and mortality in observational studies. A platelets to O individuals is similar and we got that wrong. Worry about the anti-A in O platelets is legitimate, but less important than worrying about what happens when you have circulating platelets (and immune complexes) coated with loads of IgM and IgG antibody. Bleeding at a rate of 70% in the PLADO study. Our bleeding rate avoiding ABO mismatching is about 1-3%.
Avoiding infusing ABO antibody to the recipient’s cells and donor cells is also a worthwhile struggle. Remember that it isn’t only red cells that carry ABO antigens. It’s platelets, endothelial cells, hepatocytes, etc. So avoiding infusing anti-A from an O platelet or red cell donor into an A or AB recipients is worth doing. We do this, when necessary by removing supernatant plasma from group O red cells and platelets by (Oh My God) washing. It’s cheap (when using a floor centrifuge), doesn’t take a great deal of time and reduces toxic anti-A and anti-B by 95%. In our hands, this improves survival in acute myeloid leukemia in selected patient subsets.
Washed O platelets and red cells are truly universal donor, unlike the red cells which contain a few dozen milliliters of plasma, which adds up over multiple transfusions, and, rarely, causes serious hemolysis.
I know this conflicts with long standing dogma, but we’ve got data rather than dogma :).
Thanks for all your work Joe. Lots to digest in the podcast and rather timely given recent discussions at my place of work.
This episode DID have a lot of information, Clare! Glad it was helpful.
-Joe