FACT: There is a good chance you’ve never actually seen acquired B in real life (and never will).
FACT: If you work in a laboratory, Murphy’s Law says you will come across your first ABO type discrepancy such as acquired B precisely three minutes before your shift ends or in the last seconds before it’s time for your lunch break. Thanks, Murphy.
FACT: If you take any type of exam containing blood banking questions at any point in your life, you will be asked questions pertaining to acquired B.
Acquired B is one of the more popular topics for those looking for weird things in the ABO system about which to write exam questions, and it has befuddled those learning immunohematology for decades. But it’s not just an “exam thing!” Blood banking professionals should understand acquired B clearly, because it can happen in everyday practice, and as we will see, it may be a clue that a patient has a big problem. So let’s do this!

Basic ABO Grouping
Routine ABO testing is performed in two distinct (but usually simultaneous) stages, known as “red cell grouping” (blood bankers more commonly call it “forward grouping” or the “front type”) and “serum grouping” (“reverse grouping” or the “back type”). In red cell grouping, not surprisingly, the laboratorian uses very powerful monoclonal reagent anti-A and anti-B to determine if either A or B antigens (or both) are present on the red cells of the person being tested. When performing serum grouping, on the other hand, the worker uses the patient’s serum (or plasma) and reacts it against laboratory cells of A1 and B types. Red cell grouping identifies which ABO antigens are present on the person’s red cells, while serum grouping identified which ABO antibodies the same person carries.
Note that some facilities (and some geographic regions) add additional reagents, potentially to either red cell or serum grouping. Some test the red cells with anti-A1 or anti-A,B in addition to anti-A and -B, but generally, these reagents are not necessary for routine typing (they may be more useful with weak ABO antigen expression). In addition, some add testing of the serum against group O RBCs; again, this is generally not necessary for routine testing.
Here’s an example of how it works: If a person’s red blood cells (RBCs) react strongly with reagent anti-A but not anti-B, we would interpret their red cell grouping as blood group A. That same person’s serum should have no reaction with reagent group A1 RBCs and strong reaction with reagent group B RBCs (demonstrating the expected presence of anti-B in the serum). Thus, the serum grouping interpretation would also be blood group A. If the interpretations match, we all can say “yay!” and move along with our day (see this illustrated in the figure below).
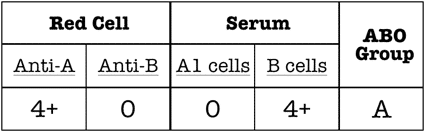
Typical appearance of ABO testing for a group A person
Basic ABO Antigen and Antibody Stuff
The ABO sugars for group A and group B are not really all that different. They are built on the same long sugar and protein (“glycoprotein”) “type 2 chains” on the red cell surface, and the only difference between them is the very last sugar that is attached to the long chain. This sugar, known as the “immunodominant sugar,” is N-acetylgalactosamine (Gal-NAc) for group A, and galactose (Gal) for group B (see image below). Just one little sugar makes all the difference.
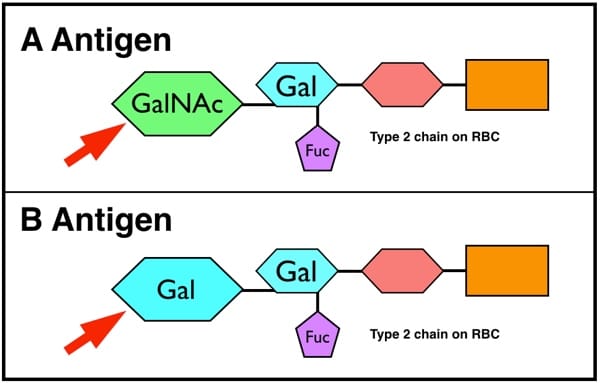
GalNAc=N-acetylgalactosamine
Gal=Galactose
Fuc=Fucose
Acquired B: What Happens?
Usually, acquired B occurs when the RBCs from a blood group A patient come in contact with bacterial enzymes known as “deacetylases” carried by bacteria that live in the colon (typically gram-negative rods). No, this is not a normal state of affairs, and before I get into the mechanics of what this type of exposure can mean for an individual’s RBC forward typing results, let me point out that this is one of my favorite examples of how lab folk and clinical folk can help each other. The interaction of bacterial enzymes and red cells most commonly occurs when the patient has something significant (and BAD!) happening in his or her lower GI tract, such as colorectal cancer or a colonic obstruction, or in the face of developing or established gram-negative sepsis. It is possible that the discovery of acquired B may be the first indication that a patient has a serious issue (such as colon cancer that is not yet evident). Blood type testing can be an important window into a patient’s overall health, and can give information to a clinician indicating serious medical issues.
Now, back to what these bacterial enzymes do to an individual’s blood type. Activity of these enzymes results in removal of the acetyl group from the residue that gives the A antigen its specificity, N-acetylgalactosamine (GalNAc). This modification leaves the A-specific sugar as galactosamine (N-acetylgalactosamine with the acetyl group removed = galactosamine). Recall that normally, the group B-specific sugar is galactose.
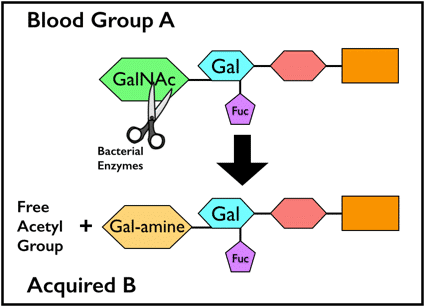
Acquired B biochemistry. Note the scissors “cutting” the acetyl group away from GalNAc
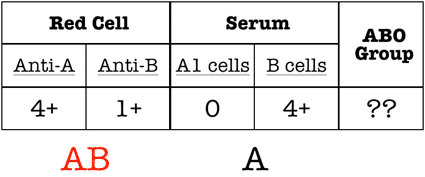
Note the “extra” reaction in the red cell grouping. This is an ABO discrepancy.
It is important to recognize, however, that this “acquired B” is NOT a real-live B! Galactosamine is not the same as galactose, and while some monoclonal anti-B reagents will recognize it as such, the patient’s own strong, healthy anti-B just turns up its nose at the acquired B! Obviously, if the enzyme modification led to formation of actual B antigen, the patient’s own anti-B would cause hemolysis in a big, ugly way, and we don’t see that at all.
Figuring it Out
So, what does this actually mean? How do these patients actually get transfused? This is where the recognition of the entity in a transfusion service or reference laboratory is essential. Several simple strategies can be employed to prove that this patient is really NOT group AB. It’s important to note, the acquired B phenotype is a transient condition. Over time, when the root cause of the bacterial enzyme removal of the acetyl group is resolved, a patient’s blood type will no longer show an acquired B antigen.
First, I always advise people to check the patient’s diagnostic history! As mentioned above, the rare cases of acquired B that are still seen will usually be associated with colorectal malignancy, gastrointestinal obstruction, or gram-negative sepsis (where those bacteria can contact the RBCs).
Second, adding the patient’s own serum to his RBCs (autoincubation) reveals no incompatibility. In other words, this patient’s own very strong anti-B does not recognize the acquired B antigen (which is really just a partially modified group A antigen) as being an actual group B antigen. We already know that this patient has anti-B in his serum from his serum grouping results (see above), but the patient’s own anti-B completely ignores the acquired B antigen on his RBCs (even though human anti-B from other people will react). This is an important distinction between an ABO discrepancy caused by acquired B and one caused by a cold-reacting autoagglutinin, which we will discuss more in a future presentation about ABO discrepancies.
Third, the technologist can use a different form of monoclonal anti-B in the patient’s red cell grouping test. Certain clones are known to react with acquired B, while others are not (normally specified in the package insert), and choosing a different clone (often easier in reference lab settings than in hospital settings where only one anti-B type is stocked) will render the forward grouping consistent with that of a group A person. Some countries (the United Kingdom, for example) have specified that monoclonal anti-B that recognizes acquired B RBCs should not be used at all!
In addition, incubating the acquired B RBCs with acetic anhydride will lead to “re-acetylation” of the modified A antigen and loss of the B-like activity. Finally, acidifying the reaction mixture of the patient’s RBCs with human anti-B (non-self) can eliminate the incompatibility with that source of anti-B.
In the end, acquired B is a serologic problem that is fairly easy to recognize, especially on examinations. In real life, experienced blood bankers can diagnose and confirm Acquired B fairly easily. These patients can receive group A blood without a problem, and the ABO discrepancy will disappear as the infection or other situation causing causing contact with bacterial enzymes clears.
The acquired B phenomenon is an interesting one, as it is an insightful indicator linking lab serology with clinical diagnosis. And yet, whether you agree it’s “interesting” or not is irrelevant because it is simply one of those blood bank occurrences you will need to know for any blood banking exam you take. I always tell those preparing for exams that when they see a question that starts with words like, “A 73 year old male with colon cancer…,” they should immediately check the answer for acquired B!
If you’ve seen an interesting case of acquired B in your patient care experience or laboratory practice, or have additional insight to share on this strange little beastie, I’d love to read your comment below.
For additional information, or to see this situation illustrated, you can check out the video I made on Acquired B in 2014. Future posts will cover another “weird” ABO-related issue, the Bombay Phenotype, and I plan to do a presentation on ABO discrepancies in general eventually (perhaps when I acquire that “nerd” mutation I mentioned at the beginning!).














our teacher give us an assignment about the same case. we are very worried about that after reading of this page.i am solve all the teacher question..i shall be very thankful to you
What substances will be detected in his secretions?
For someone with acquired B (remember, that person is actually group A), the secretions will be what you would normally expect for a group A person. That is, 80% will express both H and A antigens, while 20% will express neither in the secretions. This is not a genetic change, but a mechanical modification of antigens in the blood coming in contact with bacterial enzymes, so the secretions are unaffected.
-Joe
Once treated for the cancer or bacteria, do their red blood cells regain the blood group antigens and test normal again.?
Just want to say ” Thanks for all you do!”. It’s a great help 🙂
You are most welcome, Leslie!
-Joe
Here is a question that I discussed with a student of mine lately.
We know that antibodies are developed against an antigens.
For a Group O individual, there are No A or B antigens on their eryhtrocytes.
So how come this individual has both anti-A and anti-B antibodies??
Well, that is pretty much the point in the ABO system, Emory: People develop antibodies against the antigens they lack on their red cells. Don’t get hung up on the fact that they haven’t seen A or B antigens on other RBCs, specifically, because it appears that the ABO antigens are present throughout nature (like in bacterial cell walls, for example), and we see them just by being alive and outside of our mothers’ womb.
-Joe
I am A positive but noticed on some labs of mine that it says A, Permanent ABO discrepancy. What does that mean for me in relation to your article/lesson. I’m very curious. Thanks
Hard to tell, Vaness. You would need to discuss with the medical director of the lab that did the testing (or a representative), as what you wrote could have one of many meanings. Sorry I can’t help more!
-Joe
Thank you for this content-rich website. It’s very helpful for me.
I have a question about B(A) when it is found in a donor or a patient who is scheduled collecting autologous blood.
Is there any risk of infection? Do you know any case of TTI from B(A) blood?
Does this “acquired” phenomenon resolve itself? -Or is it a permanent change?
Andrea, it DOES typically resolve itself.
-Joe
I was A+ for most my life. I had several blood type tests from birth all the way up to my 20’s. When I got married, you can imagen my surprise when I can out B+.
I got re-tested 5 times more, all came out B+. My medical history contradicts the test results.
14 years after the test, I’m still B+, never been sick a day in my life, and still no answer as to how or why I’m now B+.
I’ve only taken antibiotics once in my life (strep throat).
Any clues on how I can find an answer? Should I be worried?
Here’s a neat “Acquired B” 2019 case study, an A becomes an AB. Thankfully very sick baby recovers.
It’s from the Department of Transfusion Medicine, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh-160012, India
Acquired-B phenomenon in a neonate presenting with necrotizing enterocolitis Transfusion and Apheresis Science
Volume 58, Issue 1, February 2019, Pages 30-31
https://www.sciencedirect.com/science/article/abs/pii/S1473050218303781
RH A negative on front and no anti-B on the back? What does it mean?
will there be any reaction if a patient with bod group A showing Acquired B Phenomenon receives Blood Group A plasma? Like will Anti-B react with the Acquired B Ag on patient’s RBCs? Will it be a major reaction?
Acquired B is not a “real” phenomenon, Tan. In other words, the person with acquired B is really blood group A, and should react exactly like a blood group A person would. Specifically, the anti-B in such a person’s plasma does not react with acquired B RBCs.
-Joe
I’ve lived with O- blood type for most of my life, including my baby card. However, the other day I had a test done and learned that I have AB+ blood, and a week later I had a test done and learned that I have AB+ blood type again.
I’d suggest discussing this with a local transfusion medicine expert. You may have to search, and potentially work through either a hematology physician or local pathologist, but there are reasons this could have happened, and only someone who can work with you directly could potentially get to the bottom of something like this. I wish you the best.
-Joe