Most blood bankers really dislike ABO discrepancies, but Nicole Draper says, “They’re not so bad!” She teaches three simple rules that will get you on the road to solving most of these cases quickly.

Dr. Nicole Draper
Getting the Most From This Episode
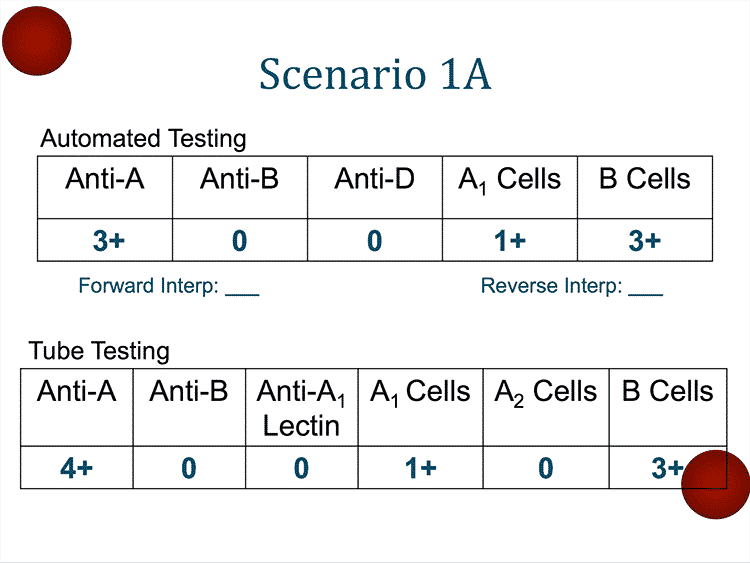
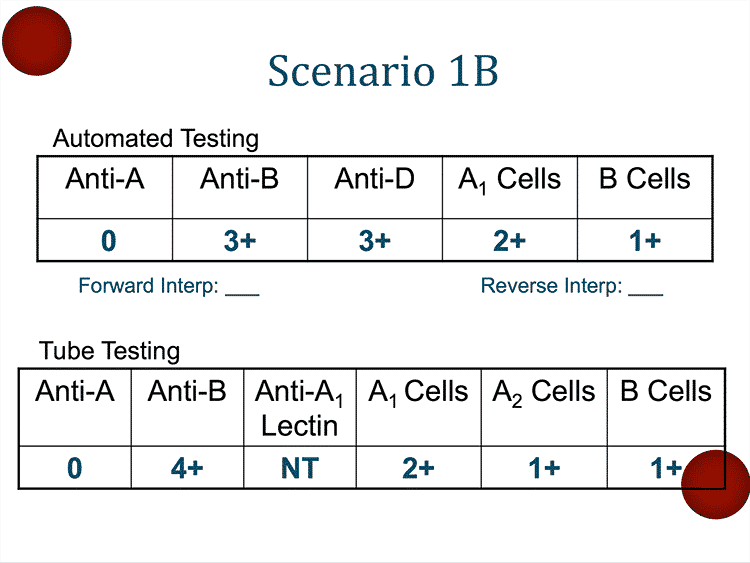
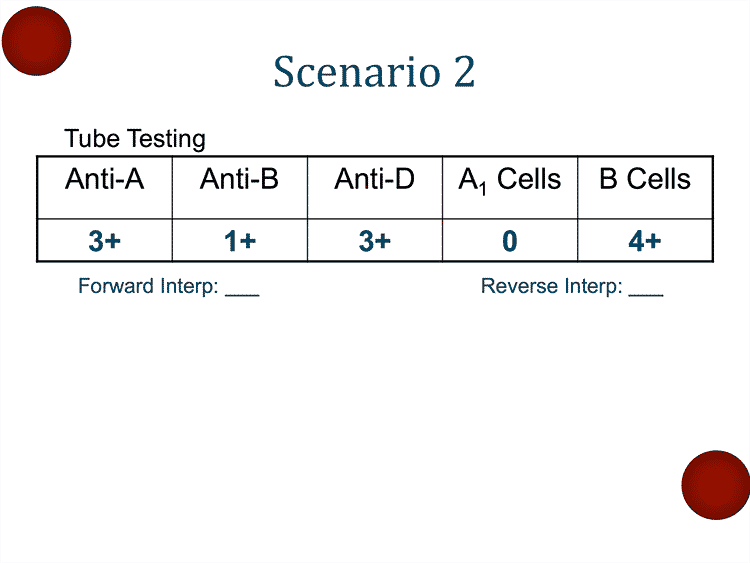
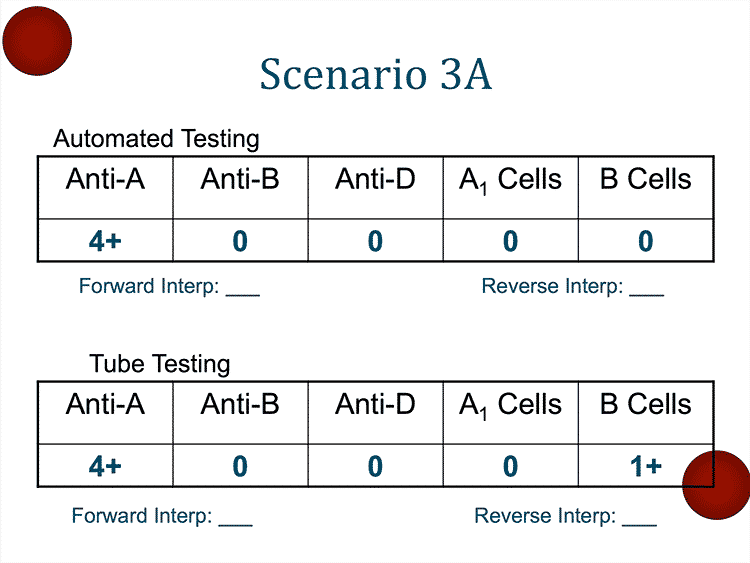
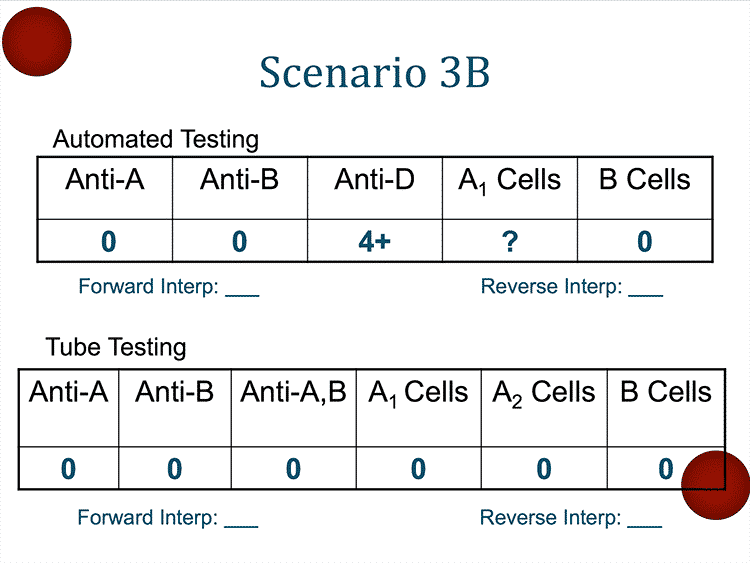
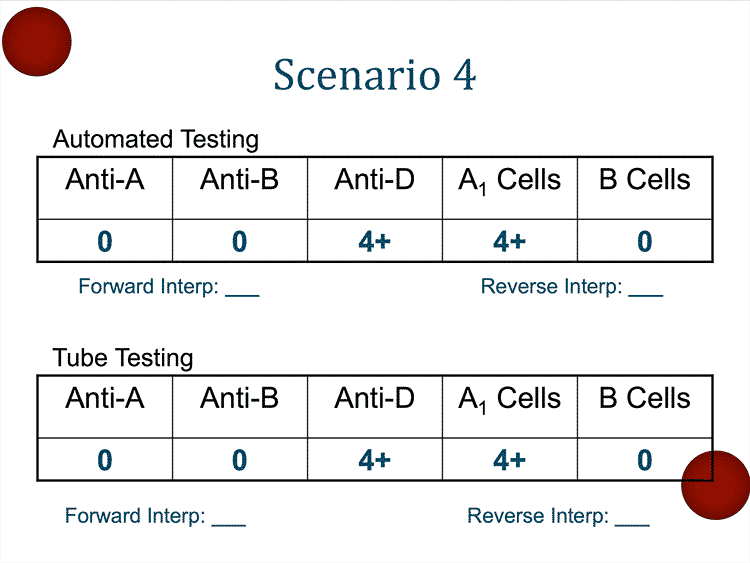
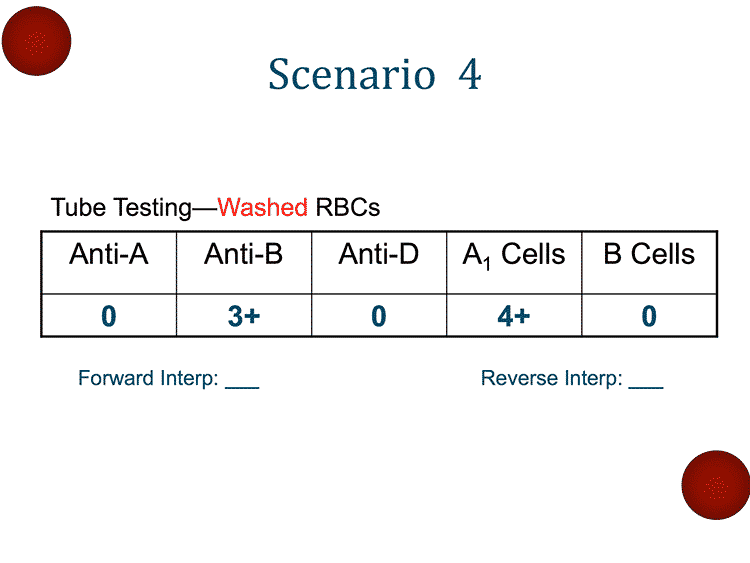
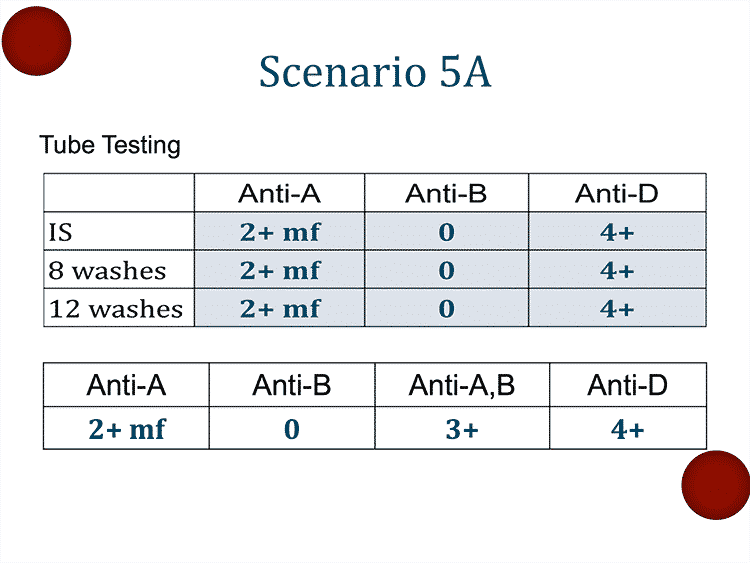
Like many topics in immunohematology, the evaluation of ABO discrepancies is very visual. For that reason, the best way to listen to this episode is with the cases printed out or viewed on your computer, tablet, or mobile device screen. You can find everything you need to visualize what Dr. Draper describes in the interview further down on this page. My advice: Print out the handout and have it in front of you so you can try to solve the cases along with Dr. Draper.
Also, if you feel lost in just understanding the basics of ABO testing, so this episode feels completely beyond you, start by reading my blog post on the essentials of ABO testing, then come back and try listening to this episode.

Dr. Nicole Draper
Getting the Most From This Episode
Like many topics in immunohematology, the evaluation of ABO discrepancies is very visual. For that reason, the best way to listen to this episode is with the cases printed out or viewed on your computer, tablet, or mobile device screen. You can find everything you need to visualize what Dr. Draper describes in the interview further down on this page. My advice: Print out the handout and have it in front of you so you can try to solve the cases along with Dr. Draper.
Also, if you feel lost in just understanding the basics of ABO testing, so this episode feels completely beyond you, start by reading my blog post on the essentials of ABO testing, then come back and try listening to this episode.
-Weakest reactions are usually discrepant
-Antibody problems are much more common than antigen problems
About My Guest:
Nicole Draper, MD, is an Associate Professor of Clinical Practice in the Department of Pathology at the University of Colorado School of Medicine. She is the Associate Director of Transfusion Services at the University of Colorado Hospital in Aurora, CO, and helps direct numerous other transfusion services in throughout the Denver area in the CU system.
Nicole is a graduate of the University of Utah School of Medicine, and completed her Blood Banking/Transfusion Medicine Fellowship at Puget Sound Blood Center (Now Bloodworks) in Seattle, WA. She is a six-time winner of the “Summit Award for Pathology Resident Teaching” at CU, and has given presentations on ABO discrepancies at the AABB Annual Meeting in 2013 and 2016.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. Neither Dr. Draper nor I have any relevant financial disclosures.
The images below are generously provided by Dr. Draper. Click on an image to see a larger version. You may also click here to download a pdf version of these images to print or use to follow along.
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














Amazing episode, Nicole. Thanks Joe, for bringing it to us despite your “lack of interest” in this subject 😉 I think you were a wonderful host. And this work you do is absolutely stunning! I enjoy it a LOT!
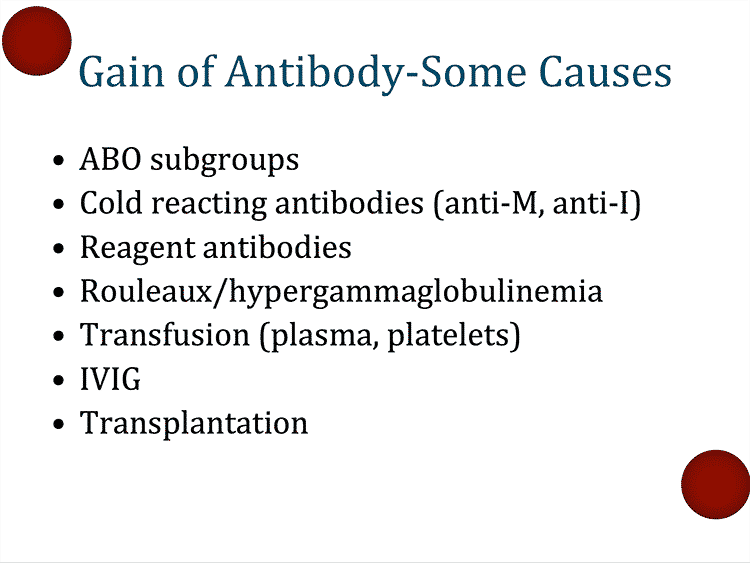
Very useful the 3 rules Nicole mentioned here: patients history, weak reactions are usually discrepant reactions and antibody problems are more common than antigen problems. I will bring them with me from now on.
I was wondering about the case of the patient with hypergammaglobulinemia. Nicole said you could use DTT to denature the IgMs by cutting their disulfide bonds. But wouldn’t that make disappear the reaction of the “natural” anti-A as well?
Once again, thank you so much.
Greetings
Mariana
That’s a good question concerning Mariana? I am interested in the answer.
Why wasn’t saline replacement used?
That was my thought as well, Rouleaux should be addressed with saline replacement yes?
Thanks a lot, Dr.Nicole Draper for an excellent podcast. I have been working in blood bank for the last ten years. So I am familiar with most of the scenarios but there are some very important points that I learned today e.g:
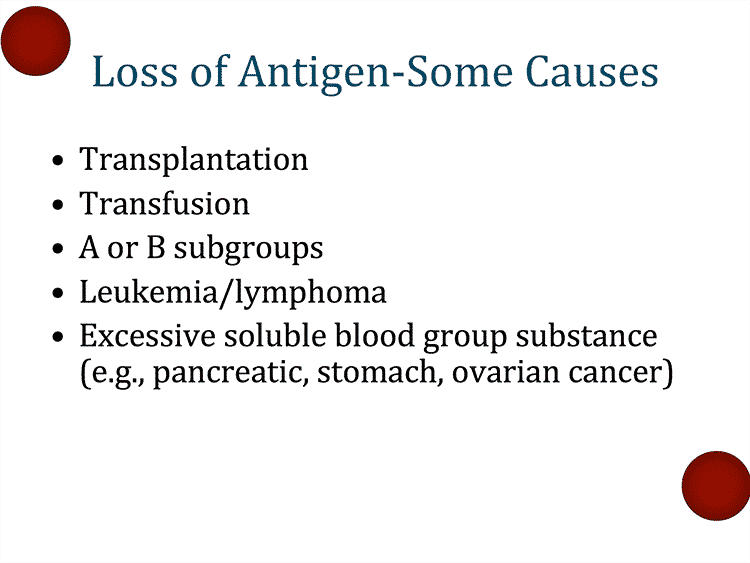
Usage of anti-A,B for forward group problem resolution
correlation of IGM levels with Grouping
and the increase of blood group substances in certain type of cancers.
Thank you for this simplified and super comprehensive podcast,Drs Chaffin and Draper. I tell people that blood bank test discrepancies may really really help support clinicians in patient management. Many times, these possibly ‘clinically significant discrepancies’ are resolved ONLY for the purposes of providing blood products for transfusion.
Thanks for your podcast . They are very helpful .
I see in #4 that washing brought up the B type, but, at the same time, the reaction with Anti-D went from 4+ to 0, is this a typo or did I miss something?
You did not miss anything, Elaine! You are correct; it’s a typo. My apologies.
-Joe
Thanks for the quick reply; I have to say, I get a lot of useful info from your podcasts,
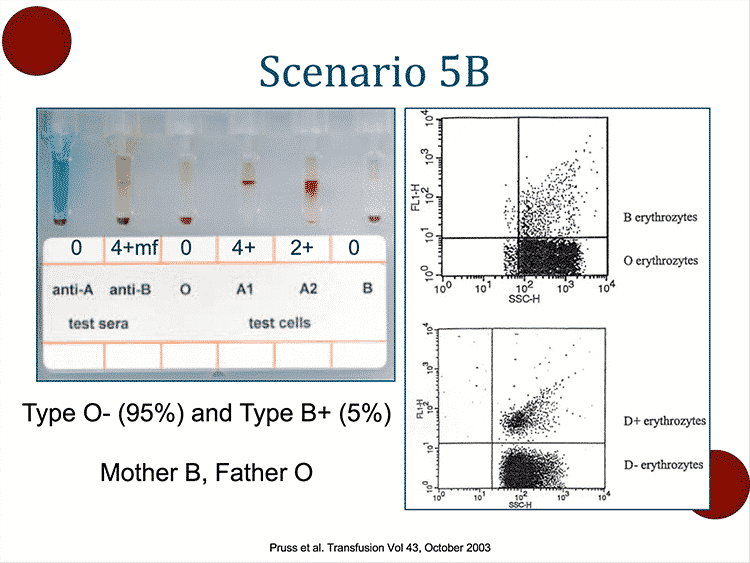
with the last chimera case, what would you suggest to transfuse, RBC and FFP? Do we go by the rules used for transplant patients?
Joe, Thank you for all the great examples and information that comes through the podcasts. I would just like to comment regarding the O,B chimera example Scenario 5B- it is true that chimeras may develop normally and then be seen later in life as a phenomenon that somehow “tricks” or “gets under the radar” of the immune system. I think more accurately, it should be noted that the late development of the immune system compared with our structural development is what allows the immune system to accept chimeric features as our own (self) so that antibodies are not made to cell products exposed to over a lifetime.
I apologize for still posting questions under this 2018 podcast in 2021. However I have a general question. What is the difference between tube testing (or tile testing) and automated testing, and why is tube testing more sensitive than automated?
Not sure that “more sensitive” is accurate, Vivian. Instead you might say that tube testing can be more easily manipulated to enhance ABO reactions (by doing things like incubating in cold temperatures and using different forms of antibodies to test, etc.). Those manipulations can enhance reactions and bring out reactions that might not have been visible using “standard” techniques.
-Joe
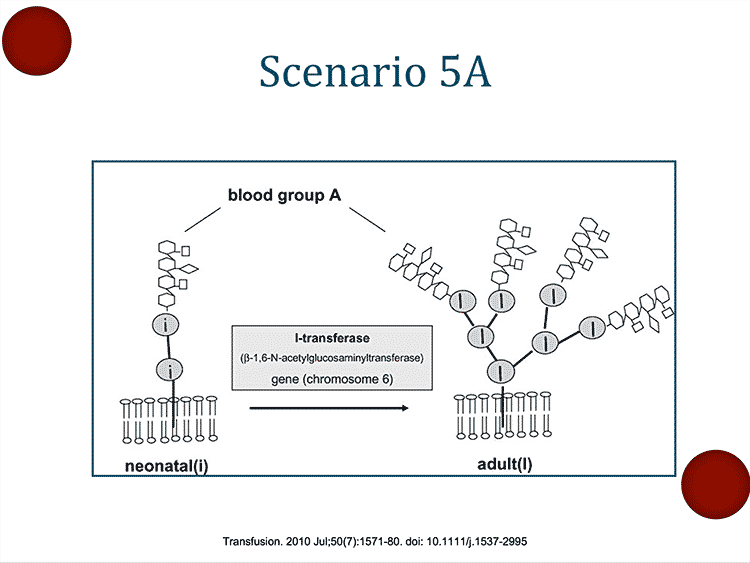
Very sorry if I missed the explanation. But with scenario 5A, why did the anti-A,B not produce a mf reaction?
Given that the baby has a weak ABO expression, why does using anti-A,B instead of anti-A produce a more consistent result?
Yeah I was wandering the same thing!
I can’t thank you enough for this podcast! I work in a small transfusion department in Eastern Europe, we still use a-A,B test-serums here and I’ve always wondered why the western literature describes front typing with only a-A and a-B. Your podcast made everything so clear! I’ve got a question though – do you guys use an autocontrol for the blood group typing – a droplet of patient’s RBCs and a bigger drop of the patient’s plasma. If yes – what could cause agglutination in the autocontrol, and if not – why don’t you use it?
Amazing podcast, thank you!
Hello great podcast 🫡
Why there was 3+ reaction with anti A,B in scenario 5A?
Regards