“Oh, no! There’s an isolated reaction that we can’t explain!” Brenda Grossman helps you understand what these reactions are, and what they might (or might not) become.

Dr. Brenda Grossman
Data, Please!
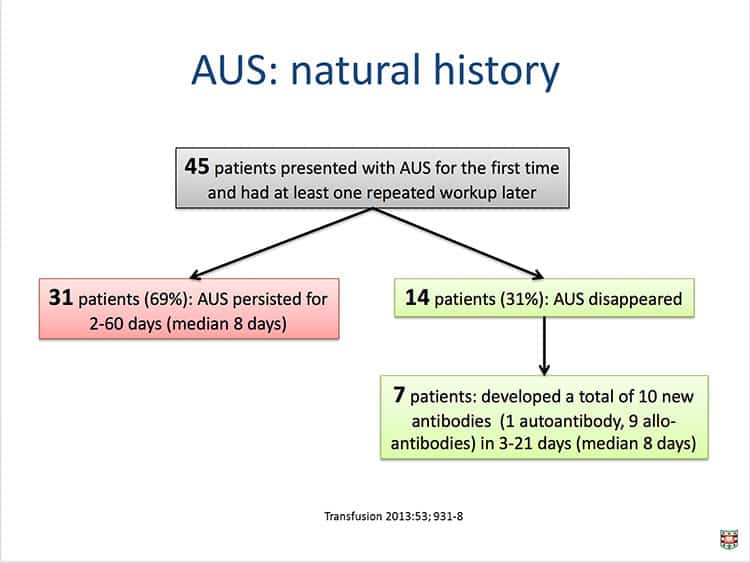
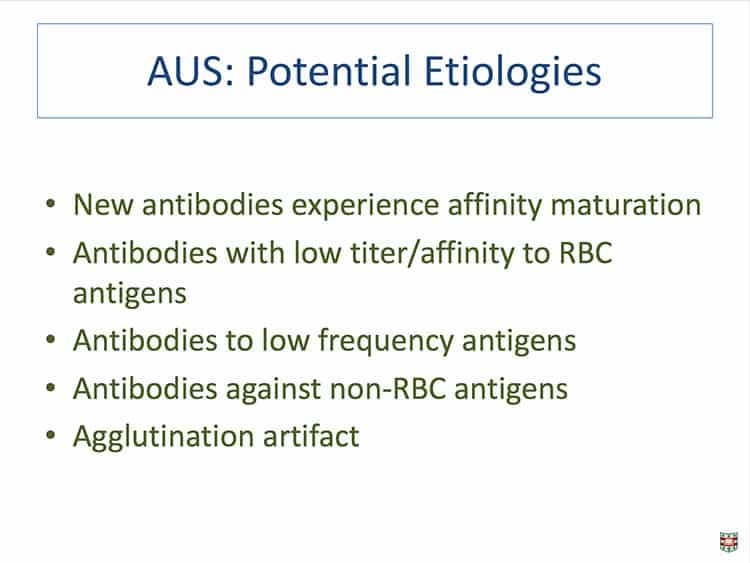
Dr. Brenda Grossman has been there, and she feels your pain! Brenda was trying to explain these isolated reactions to one of her residents a few years back, and it dawned on her that solid data on these “antibodies of undetermined specificity” (as she came to describe them) was pretty much nonexistent. So, she and that resident (and later colleague), Dr. Chang Liu, put together a study describing the frequency of these irritating “stray” reactions in a large cohort of patients at their hospital in St. Louis. What they found may surprise you (put it this way: The most common antibody they identified in their study was not anti-D, anti-E, or anti-K, as you might guess!). Brenda also outlines some possible management strategies for patients impacted by antibodies of undetermined specificity.

Dr. Brenda Grossman
Data, Please!
Dr. Brenda Grossman has been there, and she feels your pain! Brenda was trying to explain these isolated reactions to one of her residents a few years back, and it dawned on her that solid data on these “antibodies of undetermined specificity” (as she came to describe them) was pretty much nonexistent. So, she and that resident (and later colleague), Dr. Chang Liu, put together a study describing the frequency of these irritating “stray” reactions in a large cohort of patients at their hospital in St. Louis. What they found may surprise you (put it this way: The most common antibody they identified in their study was not anti-D, anti-E, or anti-K, as you might guess!). Brenda also outlines some possible management strategies for patients impacted by antibodies of undetermined specificity.
About My Guest:
Brenda Grossman, MD, MPH is a professor in the Department of Pathology and Immunology and the Department of Medicine at Washington University in St. Louis, MO. She is board-certified in Internal Medicine, Hematology, and Blood Banking/Transfusion Medicine. She serves as Medical Director of Transfusion Medicine Services at Barnes-Jewish Hospital, and is the program director for both the Clinical Pathology Residency Program and Transfusion Medicine Fellowship at Washington University. Brenda served as associate editor for the 16th, 17th, and (current) 18th editions of the AABB Technical Manual. She has won numerous teaching awards, and has numerous publications in peer-reviewed journals including Transfusion, JAMA, Vox Sanguinis, and the Annals of Internal Medicine.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. Neither Dr. Grossman nor I have any relevant financial disclosures.
The images below are generously provided by Dr. Grossman.
Further Reading:
- Dr. Grossman and Liu’s article discussed in this interview: Liu C and Grossman BJ. Antibody of undetermined specificity: frequency, laboratory features, and natural history. Transfusion 2013;53:931-938.
- Editorial accompanying the above article: Tormey CA and Hendrickson JE. Antibodies of undetermined significance: nuisance or near miss? Transfusion 2013;53:926-928.
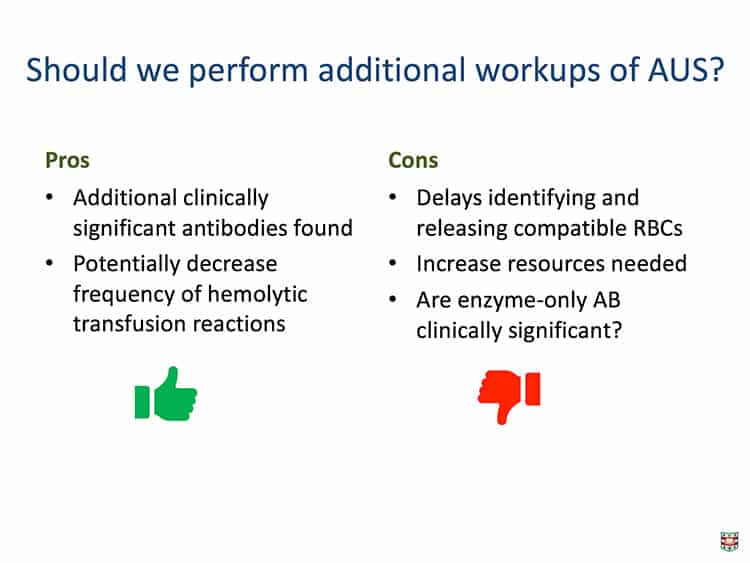
- Study Dr Grossman mentioned, using ficin treatment to resolve AUS: Hill BC et al. Ficin-Treated Red Cells Help Identify Clinically Significant Alloantibodies Masked as Reactions of Undetermined Specificity in Gel Microtubes. Laboratory Medicine 2017;48:24-28.
- Later study with similar results in solid-phase testing: Miller NM et al. Patient factors associated with unidentified reactivity in solid- phase and polyethylene glycol antibody detection methods. Transfusion 2017;57;1288–1293.
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














Another absorbing podcast; thank you both.
As you may know, in the UK we would almost automatically perform a panel with enzyme-treated red cells (usually papain, rather than ficin), although, these days, the reference centres are using the papain-IAT method in column agglutination technology, as we find we get “crisper” reactions, however, without a doubt, performing these tests routinely certainly means we detect fewer antibodies that we genuinely cannot identify a specificity (although, of course, we still get some).
Others listening to this excellent podcast may be interested in another paper published some years ago now (Sachs UJH, Röder L, Santoso S, Bein G. Does a negative direct antiglobulin test exclude warm autoimmune haemolytic anaemia? A prospective study of 504 cases. British Journal of Haematology 2006; 132: 651-661) that, on the face of it doesn’t have much in common with this podcast, but actually does!
As a serologist myself, I was always less worried about AUS in the samples from patients who required a transfusion, than I was in patients who were pregnant, in case we were “missing” an antibody directed against a low prevalence antigen, in a pregnancy where the foetus had inherited the gene leading to the expression of this antigen from the father.
A REALLY interesting podcast.
Thank you, Malcolm. I appreciate your perspective, as always, and thank you for filling in some details on how things are done routinely in the UK.
-Joe
Thank you, Dr. Brenda Grossmanand Joe. Another excellent podcast. AUS-18%, that means a significant chunk of time the blood bankers spend in figuring these antibodies out.
Time plays a crucial role in how far we go hunting these down. That’s why probably the reference lab and hospitals deal with these in different ways. Nobody likes to delay or cancel the surgeries/treatment due to AUS unless you are suspecting something clinically significant. That’s why an IAT cross-match is the best option for these situations.