Platelet transfusions are life-saving in many situations, but what do you do when they might NOT be helpful?

Dr. Ruchika Goel
But What About ITP, TTP, and HIT?
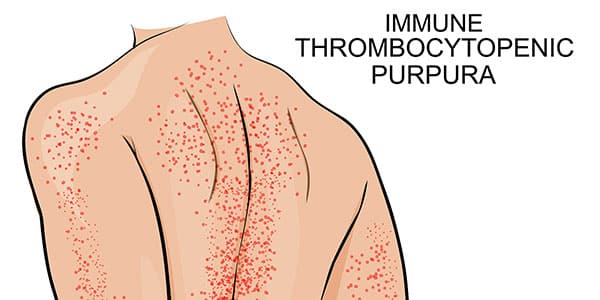
Despite the truth of the statements above, we have wondered for decades about whether or not platelets should be given to patients with certain diseases where their platelets are being removed from circulation. Patients with those diseases, most famously ITP (Immune Thrombocytopenic Purpura), TTP (Thrombotic Thrombocytopenic Purpura), and HIT (Heparin-induced Thrombocytopenia), might not respond at all to platelets. More concerning, some of those patients might actually be harmed by platelet transfusion!
Let’s Go to the Data
My guest in this episode, Dr. Ruchika Goel, looked carefully at US data on platelet transfusion in ITP, TTP, and HIT, and she has some insights that might change the way you transfuse these patients.

Dr. Ruchika Goel
But What About ITP, TTP, and HIT?
Despite the truth of the statements above, we have wondered for decades about whether or not platelets should be given to patients with certain diseases where their platelets are being removed from circulation. Patients with those diseases, most famously ITP (Immune Thrombocytopenic Purpura), TTP (Thrombotic Thrombocytopenic Purpura), and HIT (Heparin-induced Thrombocytopenia), might not respond at all to platelets. More concerning, some of those patients might actually be harmed by platelet transfusion!
Let’s Go to the Data
My guest in this episode, Dr. Ruchika Goel, looked carefully at US data on platelet transfusion in ITP, TTP, and HIT, and she has some insights that might change the way you transfuse these patients.
About My Guest:
Dr. Ruchika Goel is an Associate Professor of Internal Medicine and Pediatrics, Division of Hematology/Oncology at the Simmons Cancer Institute at Southern Illinois University School of Medicine and an Adjunct Assistant Professor of Pathology in the Division of Transfusion Medicine at Johns Hopkins University. In addition, she serves as the Medical Director of ImpactLife, formerly known as the Mississippi Valley Regional Blood Center.
Dr. Goel is a practicing hematologist/oncologist as well as a transfusion medicine physician, and she is actively engaged in research in Big Data applications in Transfusion Medicine and Pediatric and Neonatal Transfusions. She is the current chair of the Pediatric Subgroup of the International Society of Blood Transfusion (ISBT) and a participating member of the AABB Standards committee. She also serves as an invited consultant for REDS IV-pediatric longitudinal studies.
Dr. Goel has multiple accolades and awards to her name including the AABB Fenwal Annual Transfusion Medicine Scholarship Award, Paul J Stranjford Young Investigator award by the American College of Laboratory Physician and Scientists and has also received international recognition with the ISBT 2016 Harold Gunsen fellowship award.
Dr. Goel has over 70 peer reviewed publications to her name including key first author publications in some leading journals including JAMA, JAMA Surgery, Blood, Transfusion and Vox Sanguinis and has been invited to lecture nationally and internationally on topics of her research focus.
DISCLAIMER: The opinions expressed on this episode are those of my guest and I alone, and do not reflect those of the organizations with which either of us is affiliated. Neither Dr. Goel nor I have any relevant financial disclosures.
Further Reading:
- Main article discussed, on transfusion in ITP: Goel R et al. Platelet transfusion practices in immune thrombocytopenia related hospitalizations. Transfusion 2019;59:169-176.
- MedPage Today Article: MedPage Today discussion of the above article regarding overuse of platelets in ITP.
- 2015 article outlining possible danger from platelet transfusion in TTP and HIT: Goel R et al. Platelet transfusions in platelet consumptive disorders are associated with arterial thrombosis and in-hospital mortality. Blood (2015) 125 (9): 1470–1476.
- 2019 American Society of Hematology ITP Treatment Guidelines: Neunert C et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv 2019;.
Thanks to:
- Samantha Chaffin, Design and content consultant
Music Credit
Music for this episode includes “Cuando te invade el temor” and “Reflejo,” both by Mar Virtual via the Free Music Archive. Click the image below for permissions and license details.














Nice discussion. There are many situations where platelet transfusions may be doing more harm than good. Like many pro-hemostatic therapies, one risk appears to be thrombosis, as discussed by Dr. Goel in HIT and TTP. But thrombosis may be a more general risk as platelet transfusions are of highly activated and pro-inflammatory cells. Unfortunately, inflammation promotes both bleeding and thrombosis, so platelet transfusion may be deleterious on both counts. Particularly ABO mismatched platelets, an accepted if distinctly harmful approach.
Platelet transfusion – the new immunology of an old therapy.
Stolla M, Refaai MA, Heal JM, Spinelli SL, Garraud O, Phipps RP, Blumberg N.
Front Immunol. 2015 Feb 2;6:28. doi: 10.3389/fimmu.2015.00028.
In both therapeutic and prophylactic randomized trials, platelet transfusions is associated with with increased thrombosis and bleeding, not to mention mortality. One of our most misunderstood and misused therapeutics.
Randomized Trial of Platelet-Transfusion Thresholds in Neonates.
Curley A, Stanworth SJ, Willoughby K, Fustolo-Gunnink SF, Venkatesh V, Hudson C, Deary A, Hodge R, Hopkins V, Lopez Santamaria B, Mora A, Llewelyn C, D’Amore A, Khan R, Onland W, Lopriore E, Fijnvandraat K, New H, Clarke P, Watts T; PlaNeT2 MATISSE Collaborators.
N Engl J Med. 2019 Jan 17;380(3):242-251. doi: 10.1056/NEJMoa1807320. Epub 2018 Nov 2.
N Engl J Med 2019 Apr 18;380(16):1584. doi: 10.1056/NEJMc1902638.
Baharoglu MI, Cordonnier C, Al-Shahi Salman R, de Gans K, Koopman MM, Brand A, Majoie CB, Beenen LF, Marquering HA, Vermeulen M, Nederkoorn PJ, de Haan RJ, Roos YB; PATCH Investigators. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016 Jun 25;387(10038):2605-2613. doi: 10.1016/S0140-6736(16)30392-0. Epub 2016 May 10. PMID: 27178479.
Platelet Transfusion for PDA Closure in Preterm Infants: A Randomized Controlled Trial.
Kumar J, Dutta S, Sundaram V, Saini SS, Sharma RR, Varma N.
Pediatrics. 2019 May;143(5):e20182565. doi: 10.1542/peds.2018-2565. Epub 2019 Apr 2.
PMID: 30940676 Free article. Clinical Trial.
BACKGROUND AND OBJECTIVES: Thrombocytopenia is associated with late closure of patent ductus arteriosus (PDA). There are few studies evaluating platelet transfusions to treat PDA. We compared liberal platelet-transfusion criteria (to maintain a platelet …
It’s unlikely that three separate randomized trials showing harm are due to some quirky methodologic problem. Platelet transfusions in most or all settings except prophylaxis of bleeding at <10,000/µl are probably harmful in all likelihood. Epidemiologically they are associated with both arterial and venous thrombosis, particularly in cancer patients.
Khorana AA, Francis CW, Blumberg N, Culakova E, Refaai MA, Lyman GH. Blood transfusions, thrombosis, and mortality in hospitalized patients with cancer. Arch Intern Med. 2008 Nov 24;168(21):2377-81. doi: 10.1001/archinte.168.21.2377. PMID: 19029504; PMCID: PMC2775132.
Thank you, Dr. Blumberg!! Appreciate your inputs as well as all the references shared here. As we celebrated World Thrombosis day on October 13th, even more important to realize every single factor (especially an avoidable one) that could play a role in the complex puzzle of coagulation and thrombosis! #PlateletPBM #JustAsImportant
#PlateletPBM #JustAsImportant
Nice topic. Just wondering when will the transcript be posted?
Very soon, Hanan, I promise!
-Joe
Wonderful contribution, but Hand out needed
Hi Muben. Not sure what you mean. The transcript is now available, and the articles are linked at the bottom of the page. I hope you will check those out for more details. Thanks for listening!
-Joe